Have you noticed a strange bulge in your abdomen or groin that comes with nagging back pain?
Most people are unaware that hernias can cause back pain in unexpected ways. While you might expect pain right at the hernia site, the discomfort often spreads to your back through nerve pressure, poor posture changes, and structural displacement.
Understanding this hidden connection between hernias and back pain can help you identify the real cause of your discomfort and seek proper treatment.
I’ll show you exactly how different types of hernias trigger back pain, what symptoms to watch for, and proven methods to find relief.
Let’s learn how hernias contribute to back pain and what you can do about it.
What’s the Connection Between Hernia & Back Pain?
Yes, hernias can cause back pain, but not all hernias lead to this problem. The connection between hernias and back pain depends on the type and location of the hernia.
Signs Your Back Pain is Coming from a Hernia:
It’s not always easy to tell if a hernia causes back pain. If you only have back pain without other symptoms, another condition might be responsible. But if you have a visible bulge in your abdomen or groin along with back pain, the hernia could be the cause.
I would recommend getting checked out to determine the real cause of your back pain.
Types of Hernia
Several types of hernias can develop in different parts of your body. Each type has its own causes and symptoms. Understanding these different types helps you recognize symptoms and seek proper medical care when needed.
1. Abdominal Hernias
These are the most common groups. These happen when tissue pushes through weak spots in the abdominal wall muscles. The main types include:
- Inguinal hernia – occurs in the groin area when part of the small intestine pushes through a weak section near the groin
- Umbilical hernia – develops when part of the intestine protrudes through an opening in the abdominal muscles near the navel.
- Incisional hernia – forms at the site of a previous surgical cut
- Epigastric hernia – appears in the upper abdomen
- Femoral hernia – develops in the upper thigh area
- Hiatal hernia – occurs when part of the stomach pushes up into the chest cavity
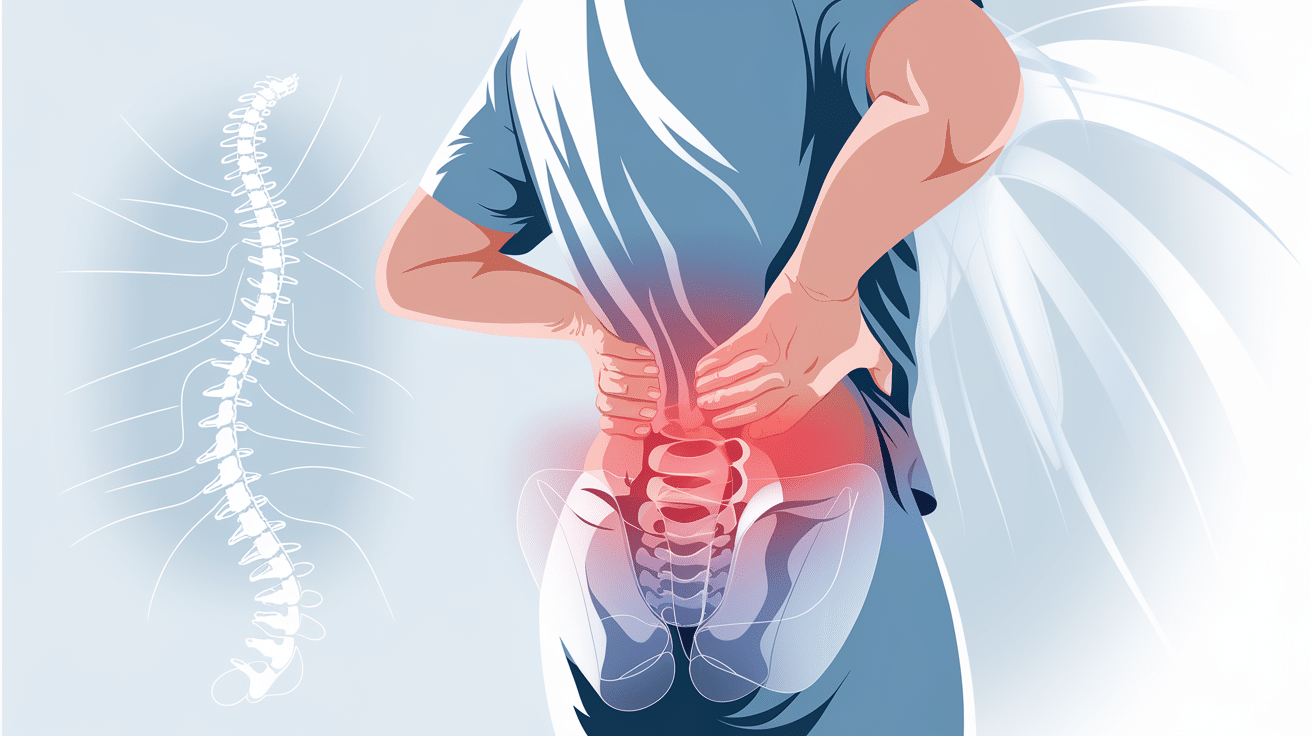
2. Spinal Hernias
These are different from abdominal hernias, also called herniated discs or slipped discs. These happen when the gel-like substance inside spinal discs squeezes out through a weak area. This can occur in the neck, mid-back, or lower back.
3. Lumbar Triangle Hernias
These are very rare. These develop in the lower back area and are less frequently documented in the medical literature.
Inguinal hernias are the most frequent type, especially in men. They can be present from birth or develop over time. Women are more likely to need emergency surgery for inguinal hernias due to complications.
The location and type of hernia affect what symptoms you experience. Some hernias cause local pain and bulging, while others can create pain that spreads to other areas, like your back.
How Does a Hernia Cause Pain in the Back?
A hernia can cause back pain in several specific ways. Understanding these connections helps explain why you might feel discomfort in your back even though the hernia is in a different part of your body.
1. Nerve Pressure: The primary way hernias create back pain is by compressing or irritating nearby nerves. When tissue or organs push through weak spots in muscle walls, they put pressure on surrounding nerves. This pressure sends pain signals that travel to your back.
This is especially true for spinal hernias (herniated discs). When the gel-like substance inside your spinal discs squeezes out, it often presses directly on spinal nerves. This creates immediate back pain and sometimes causes numbness or tingling.
2. Poor Posture: Pain from a hernia often forces you to change how you move and hold your body. You might adopt poor posture, make compensatory movements, change your walking pattern, or shift how you sit or stand.
These changes put extra strain on your back muscles and ligaments. Over time, this added stress creates secondary back pain.
3. Pain Spreading: Sometimes, hernia pain doesn’t stay in one place. The discomfort can spread from the hernia site to other areas, including your back. This happens when the hernia affects surrounding tissues and nerves or when internal structures become displaced.
4. Structural Pressure: When organs or tissue push through muscle walls, they create pressure on nearby structures. This displacement can send pain signals that you feel in your back, even though the source is elsewhere in your body.
Symptoms of Back Pain Due to a Hernia
Determining if your back pain comes from a hernia can be challenging. Healthcare professionals typically urge people to get checked out because it’s not always easy to tell.
The most important clue is having both back pain and a visible bulge. If you only have lower back pain without other symptoms, another condition could be responsible.
But if you have a bulge in your lower abdomen or groin along with pain, it may be a hernia causing this additional discomfort.
Spinal Hernia Symptoms
For herniated discs, look for:
- Pain that spreads down your arms or legs
- Pain that gets worse when you stand, sit, or move in certain ways
- Numbness, tingling, or weakness in your back, neck, or limbs
- Sharp or electric-like pain
Abdominal Hernia Symptoms
These hernias may cause back pain through:
- Visible bulge or swelling in the affected area
- Local discomfort at the hernia site
- Back pain from poor posture changes caused by a hernia, and discomfort.
When It’s Probably Not a Hernia? If you only have back pain without a visible bulge or other hernia symptoms, the cause is likely something else. Many hernias cause no symptoms or symptoms unrelated to the back.
Hernia or Herniated Disc? How to Know the Difference
Hernia or Herniated Disc: How to Know the Difference?
Understanding the difference between a hernia and a herniated disc is important since both can cause back pain but require different treatments.
What They Have in Common?
Both conditions involve something pushing through where it shouldn’t be. A herniated disc is similar in principle to an abdominal hernia: something within is trying to get out, and the result is pain.
| Aspect | Abdominal Hernia | Herniated Disc |
|---|---|---|
| Location | Abdominal wall (groin, belly, navel area) | Spine (neck, mid-back, or lower back) |
| What Pushes Through | Organs or tissues through a weakened muscle wall | Gel-like disc substance through the disc’s outer edge |
| Visibility | Creates a visible bulge or lump | Cannot be seen from the outside |
| Pain Location | Usually stays at the hernia site | Often spreads down arms or legs |
| Back Pain | May not directly affect the back | Directly causes back pain when pressing on nerves |
| Pain Severity | Localized discomfort or dragging sensation | Can range from mild backache to severe radiating pain |
| Nerve Involvement | Generally doesn’t press on spinal nerves | Often puts pressure on spinal nerves |
| Pain Pattern | Stays in one area | May spread (radiculopathy) to buttocks, legs, and calves |
How to Relieve Hernia-Related Back Pain?
- Rest and avoid strain – Skip heavy lifting, bending, or twisting movements that worsen pain.
- Take NSAIDs – Use ibuprofen or naproxen to reduce pain and inflammation.
- Apply ice packs – Use cold therapy for 15-20 minutes to numb pain and reduce swelling.
- Try heat therapy – Apply heating pads to relax muscles and improve blood flow.
- Do physical therapy – Work with professionals to strengthen muscles and improve flexibility.
- Fix your posture – Sit and stand properly to reduce back strain.
- Wear support belts – Use back braces for temporary stability and pressure relief.
- Modify daily activities – Choose gentler alternatives for tasks that cause discomfort.
When to See a Doctor ? Contact your doctor if back pain comes with a visible bulge in your abdomen or groin area.
Get emergency care for severe worsening pain, bowel troubles, urinary problems, abdominal bloating, racing heart rate, fever, nausea, vomiting, or breathing difficulties.
Conclusion
Hernias and back pain share a complex relationship that many people overlook. Whether it’s nerve pressure from a herniated disc, postural changes from an abdominal hernia, or structural displacement affecting surrounding tissues, these conditions can significantly impact your daily comfort.
The key takeaway? Don’t ignore persistent back pain, especially when accompanied by visible bulges or other warning signs. Early recognition and proper treatment can prevent complications and provide lasting relief through conservative methods like rest, NSAIDs, and physical therapy.
If you’re experiencing unexplained back pain with hernia symptoms, prioritize health and seek medical guidance.
Remember, about 9 out of 10 cases improve with non-surgical treatment, but prompt medical attention ensures you get the right care for your specific situation.
Take control of your pain today.